Speaking to History: Mental Health Policy Unit
 Takeaways
Takeaways
- Understand the circumstances and ideas that informed deinstitutionalization policies and how they shaped day-to-day practice and the lives of service users
- Identify the ways in which restrictions and discipline characteristic of the earlier long-stay mental health hospitals have been reproduced in the bureaucratized mental health and social welfare systems of the deinstitutionalization era/ that constitute community mental health
- Recognize the negative impacts of deinstitutionalization including economic and social exclusion, inadequate housing and homelessness, stigma and discrimination
 Components
Components
The components in this unit – historical documents from early community mental health and insider reflections on the era – engage in a past-present conversation about the development and ethos of community mental health in Canada. One sample of how this works is the juxtaposition of the official 1957 Saskatchewan Plan and community expert Jayne Whyte’s thoughts of the limitations of the system put into place.
More documents and reflections can be found at Components: Saskatchewan Self-Guided, Components: Toronto Self-Guided and Components: Vancouver Self-Guided.
 Evaluating the Components
Evaluating the Components
 Learning Lens
Learning Lens
The historical documents and commentaries presented in this lesson illuminate Canada’s shift from institutional to community mental health, and can be presented in lecture format by instructors or explored independently by students. Why look to the past to educate future practitioners? As anyone working in the field or using services will tell you, the merit of community mental health continues to be a topic of fervent and contentious debate. Yet this deeply contested history is largely unknown to historians, practitioners, and policymakers alike. Few know what values the original architects of community mental health saw as central to the new system, or which policy innovations were abandoned in the formative years of community mental health.
Mental health professionals work each day with the legacies of psychiatric deinstitutionalization, and holding a long view of community mental health will help them become intelligent and thoughtful practitioners. With this in mind, we handed over a set of historical documents about the deinstitutionalization plan to three people, residents of Vancouver, Regina, and Toronto respectively, whose lives have intersected with community mental health–as service users, health professionals, and activists–and asked them to share their reflections. Their thoughts, and the documents which sparked them, are presented here as a unique teaching tool, clustered geographically into three self-guided learning sections. Instructors can choose to focus on documents and audios from one region or use the entire set.
 Components in Context
Components in Context
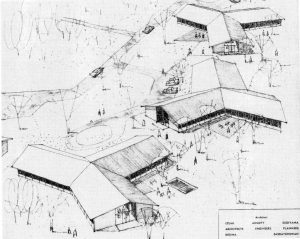
Arguably the most significant social policy in late 20th century Canada, the deinstitutionalization project saw nearly 50,000 beds closed in aging institutions across the country between 1965 and 1980, and thousands more have been closed in the quarter century since. Rippling through all sectors of Canadian society, deinstitutionalization affected the economy, the workforce, public health, social planning, education and human rights. The impact of this shift has been profound: therapeutic and professional contours of care have been re-shaped, new networks among service users have been created, and the social landscape of Canadian communities has been transformed in ways never imagined by the original architects of community mental health.
The central premise—and promise—of the shift away from the use of large mental health institutions was the integration of former patients into the life of the broader society. But the marginalization of people with psychiatric labels has continued, albeit in different forms. By the late 1970s cost-containment increasingly took precedence over social integration as the driver of deinstitutionalization. Trans-institutionalization, where patients were redistributed across a series of smaller institutionalized settings—including boarding houses, group and foster homes, nursing homes, and even jails—emerged as a new pattern. Today, mental health patients are no longer confined in long-stay mental hospitals, but their lives are now bound by the rules and restrictions of mental health and social welfare bureaucracies and in the fiscal reality of the current mental health world, the word “treatment” often appears to be a misnomer for the series of limited encounters with family doctors, community mental health teams, psych ward nurses, or police officers. Social isolation, a deeply stigmatized identity, exclusion from the work force, persistent poverty, and even homelessness, frame the lived experience of many people with mental health difficulties.


 Français
Français