Dementia Care Innovation and Moyra Jones Unit
 Takeaways
Takeaways
- Consider the diverse factors, stakeholders and processes that engender helpful innovations in mental health practice.
- Appreciate the potential of a relational dementia care model that fosters service user identity, purpose and dignity by positioning the practitioner as ally and integrating multidisciplinary rehabilitation and health care interventions
- Understand the importance of incorporating new knowledges and practices outside professional and institutional circles, allowing emergent promising mental health research and practice models to have a broad societal impact
 Components
Components
The components that underpin this unit are a set of filmed interview segments with former colleagues of Moyra Jones, a dynamic leader in Canadian dementia care. Sharing memories of Moyra, their narratives reveal a complex and caring individual and a fearless innovator. An additional component is a short home video of Jones leading a workshop in the 1990s. This video clip of community liaison Joyce Wright describing the passionate commitment of her colleague is only one of many, all of which can be found in Components: Self-Guided.
 Evaluating the Components
Evaluating the Components
- Components: Moyra Jones: Self-Guided Learning – 60 minutes
- Component Evaluation: Moyra Jones: Dementia Selfie – 15 minutes
- Component Evaluation: The Valleyview Legacy – 30 minutes
 Learning Lens
Learning Lens
Project team member Megan Davies heard about Moyra Jones from a Vancouver music therapist working in a long term care facility who recalled, “the best job she ever had,” at Valleyview, a provincial geriatric mental health facility, in the early 1980s. A health historian with research interests in mental health and old age, Davies knew that the words “geriatric”, “mental health facility” and “best ever” do not usually appear in the same sentence. Intrigued, she tracked down Jones’s former colleagues for a series of video-taped interviews and located an extensive collection of professional material left by this pioneering innovator in geriatric mental health. In the process Davies discovered some gems – the story of Canada’s first English language training program in music therapy, the beginnings of promising practices in residential dementia care, and vintage footage of Jones in action leading a workshop in the 1990s.
Other units in this module consider grassroots models of best mental health practice initiated by service users and community allies, but this historical case study explores innovation that came from within an established system, crafted and implemented by professionals and other stakeholders. Notions of innovation are often employed in economics, but here we apply the concept to dementia care, a practice field currently undergoing exponential expansion. Health care innovation is complex and involves multiple stakeholders working with existing and new ideas and practices in a transformative fashion. We ask educators and learners to think critically about professional innovation and the potential for systemic change, and to see good innovation in mental health as a collaborative process that holds the needs and dignity of service users and caregivers at the core of its vision.
Using the story of Jones and the work she inspired at Valleyview, this set of components gives future mental health practitioners an opportunity to consider the architecture of innovation and to imagine themselves as leaders in creating models of best practice. Professionally, in family care situations, and in popular culture, the way in which we regard older people with cognitive challenges reveals both deep fears of the personal and societal impacts of dementia and ageist notions of the potential and worth of the elderly. This has not shifted significantly since Moyra Jones went to work at Valleyview in 1978. Future practitioners and policy makers need to be self-reflective and to think both creatively and strategically about this field of care.
 Components in Context
Components in Context
The arc of Moyra Jones’ career spanned a vast evolution in the field of aging and mental health. In the 1950s and 1960s there was limited interest in the elderly as a social group. When the attention of Canada’s health professionals and policy analysts focused on older citizens – as the federal Senate Special Committee on Aging did in 1963 – it was to highlight the deficits of an expanding population cohort seen as largely redundant in post-World War Two Canadian society. The elderly were regarded as economically marginal individuals whose work skills were irrelevant in a modern industrial age. With an increasingly mobile population, family supports for elderly members were seen as lacking. Indeed, many health professionals considered aged grandparents to be unhealthy individuals whose brains disposed them to senility, as psychologically problematic additions to the nuclear family. The elderly psyche was regarded as similarly problematic, marked by a heightened sensitivity to loneliness, diminished self-esteem and feelings of redundancy.
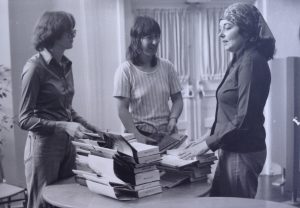
When Moyra Jones started working at George Derby, gerontology was not yet seen as a significant field of study, and pharmacological and rehabilitation treatment options for geriatric mental health difficulties were extremely limited. However, her placement in the world of veterans’ rehabilitation services situated Jones’ work alongside other innovations for former members of the military forces that were taking place elsewhere in North America. As Joy Fera, Jones’ colleague at George Derby recalled, and surviving photograph albums in Jones’ private papers illustrate, the clientele they were working with were elderly men, and this pushed the facility’s rehabilitation department to create programs suitable for an ageing male group. Their work among this group of elderly veterans brought Jones and her colleagues into contact with people with dementia, though they would not have used that term.
The unique makeup of geriatric psychiatry in British Columbia favoured Jones’ emerging interest in dementia care. From the early twentieth century, the province’s main nexus of mental health care was Essondale (renamed Riverview in 1965), a vast site in Port Coquitlam. The first facilities specifically for geriatric patients were created there in 1935 when a number of small cottages at the provincial mental health complex were set aside for their use. After World War Two this facility, modernized and renamed “Valleyview”, became the centerpiece of a provincial network of three residential geriatric psychiatry facilities: in 1948 “Dellview” opened outside the Okanagan town of Vernon and two years later “Skeenaview” was established in the northern community of Terrace. Both facilities used repurposed army camps. It appears that no other state mental health department in North America offered specific accommodation for geriatric patients at this point, making the three “Views” a unique network of institutions.
In spite of this recent modernization and expansion, by the mid-1960s Valleyview administrators were searching for ways to reduce the chronic long-term institutional population – patients who would occupy beds in the facility for their rest of their lives – and align treatment trajectories with broader plans that were emerging to deinstitutionalize mental health, at Riverview and across Canada. A 1965 Masters of Social Work thesis, coauthored by three University of British Columbia graduate students, reported that Valleyview was introducing an active research plan, conducting patient rehabilitation assessments and charging nurses with directing patients in occupational therapy techniques of resocialization and routine retraining in activities of daily living. This earlier policy initiative lay behind Jones’ mandate to transform a custodial care facility into a dynamic site for active treatment, but by 1978 it was understood that rehabilitation specialists would do the work, focusing on patients who had the potential to respond to their therapies, not the long wards of the chronically bedridden. Provincial mental health policy thus limited the number of Valleyview patients eligible for the innovative treatment options offered by the rehabilitation team that Moyra Jones assembled.
Changes in policy were matched by shifts in professional ideas about mental health in old age. During the 1970s, when Jones’ career in dementia care was taking shape, Alzheimer’s disease was being “discovered” as a major medical and social catastrophe. This is what Butler and others define as the “health politics of anguish” in a neoliberal age, whereby the social challenges of old age are regarded as medical problems and family caregivers and the aged themselves are seen as responsible for managing the presumed health risks of the senescence. Voluntary organizations such as the BC Alzheimer’s Society (1981) formed in this period to advocate and organize services on behalf of the elderly with cognitive difficulties and their families.
The work which Jones did while at Valleyview and after she left the institution maps onto these broader developments in the field of dementia care. The training films that she produced (Unraveling, The End Holds the Beginning, Love is Not Enough, Beyond Stereotypes), her public presentations, and her publications make it clear that she regarded Alzheimer’s disease and other dementias as major health issues. Indeed, Jones made biomedical explanations of these conditions a standard part of the way in which she presented her work. Where Jones’ analysis departed from a biomedical script, however, was her continued argument that, as long as there remained no “cure” for dementia, those working in the field should do their best to support people living with dementia and their caregivers, waged or voluntary. Her openness to a multidisciplinary approach was likely the result of her professional training in the University of Toronto’s joint occupational therapy/ physiotherapy program. Music therapy, a practice field that was becoming professionally organized in Canada when Jones started at Valleyview, suited her artistic and humanist leanings. It is no surprise that Jones made a film about music therapy with colleagues in Vancouver.
Moyra Jones moved on from Valleyview Hospital after less than a decade. Her subsequent contributions to the field of dementia care were considerable. In the late 1980s, with funding from Health and Welfare Canada and the British Columbia Association for Community Living, and the assistance of Joyce Wright and a myriad of community stakeholders, Jones led the Beyond Love Project, a community self-help program for caregivers that resulted in the 1991 Beyond Love Resource Book. The same year Jones was a member of the trans-Canada working group that created Health and Welfare Canada’s Design Facilities For People With Dementia. Five years later Moyra Jones Resources, based in Burnaby, brought out the first edition of GentleCare: Changing the Experience of Alzheimer’s Disease. Endorsed by gerontology specialists in the United States and Europe, the book sets out a model of dementia care that still holds currency today.
Jones described herself as an “advocate” of people living with dementia and their caregivers (bios of her books). If she were alive and active in the field today, Jones would likely be sympathetic to calls for an empowered self-identity for “forgetful people” and a vision of care as relational. The body of work which she left behind suggests that she would also have engaged with current critiques of our “hypercognitive society”, which continues to regard people with dementia as problem patients with a tragic disease.


 Français
Français